Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant
This article has been corrected.
VIEW THE CORRECTION
Abstract
Background
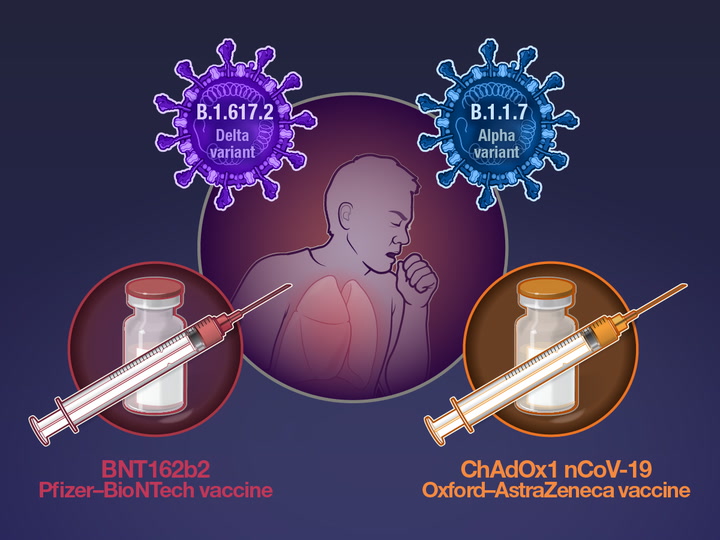
The B.1.617.2 (delta) variant of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (Covid-19), has contributed to a surge in cases in India and has now been detected across the globe, including a notable increase in cases in the United Kingdom. The effectiveness of the BNT162b2 and ChAdOx1 nCoV-19 vaccines against this variant has been unclear.
Methods
We used a test-negative case–control design to estimate the effectiveness of vaccination against symptomatic disease caused by the delta variant or the predominant strain (B.1.1.7, or alpha variant) over the period that the delta variant began circulating. Variants were identified with the use of sequencing and on the basis of the spike (S) gene status. Data on all symptomatic sequenced cases of Covid-19 in England were used to estimate the proportion of cases with either variant according to the patients’ vaccination status.

Results
Effectiveness after one dose of vaccine (BNT162b2 or ChAdOx1 nCoV-19) was notably lower among persons with the delta variant (30.7%; 95% confidence interval [CI], 25.2 to 35.7) than among those with the alpha variant (48.7%; 95% CI, 45.5 to 51.7); the results were similar for both vaccines. With the BNT162b2 vaccine, the effectiveness of two doses was 93.7% (95% CI, 91.6 to 95.3) among persons with the alpha variant and 88.0% (95% CI, 85.3 to 90.1) among those with the delta variant. With the ChAdOx1 nCoV-19 vaccine, the effectiveness of two doses was 74.5% (95% CI, 68.4 to 79.4) among persons with the alpha variant and 67.0% (95% CI, 61.3 to 71.8) among those with the delta variant.
Conclusions
Only modest differences in vaccine effectiveness were noted with the delta variant as compared with the alpha variant after the receipt of two vaccine doses. Absolute differences in vaccine effectiveness were more marked after the receipt of the first dose. This finding would support efforts to maximize vaccine uptake with two doses among vulnerable populations. (Funded by Public Health England.)
India has experienced a surge in cases of coronavirus disease 2019 (Covid-19) since late March 2021, reaching more than 400,000 cases and 4000 deaths reported each day in early May 2021.1 This increase has resulted in hospital services becoming overwhelmed and in a scarcity of oxygen supplies.2 Although only a small proportion of samples have been sequenced, B.1.617 lineages of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have dominated. The B.1.617.2 (delta) variant was first detected in India in December 2020 and became the most commonly reported variant in the country starting in mid-April 2021.1 As of May 19, 2021, the variant had been detected in 43 countries across six continents in GISAID (originally an acronym for global initiative on sharing avian influenza data but more recently a site for compiling sequence data on viruses, particularly influenza and coronaviruses, that threaten to cause a pandemic).3 In the United Kingdom, a rapid increase in cases with this variant has been seen associated with travel from India and with community transmission.4
In the United Kingdom, vaccination was initially prioritized for older adults, caregivers, and health and social care workers, with subsequent rollout to persons in clinical risk groups and younger-age cohorts.5 At an early stage of the rollout, a policy decision, based on advice from the Joint Committee on Vaccination and Immunisation, was made to use an extended administration interval of up to 12 weeks in order to maximize the number of vulnerable persons receiving the first dose during the second wave of the pandemic in the context of constraints on vaccine supply and delivery.6
Vaccines have been found to be highly efficacious at preventing symptomatic disease, as shown by clinical trials7-9 and real-world evidence.10-14 The B.1.1.7 (alpha) variant, first identified in the United Kingdom, was the predominant lineage seen between January and May 2021. Levels of protection against the alpha variant that are conferred by vaccination are similar to those observed in clinical trials, with additional protection against severe disease.10,11,15–17 Laboratory data indicate that the B.1.351 (beta) variant has reduced neutralization, according to analysis of serum samples obtained from vaccinated persons.18,19 Observational data from Qatar indicated modestly reduced effectiveness against symptomatic disease caused by this variant but high levels of effectiveness against severe, critical, or fatal disease in persons vaccinated with the BNT162b2 vaccine (Pfizer–BioNTech).17 Furthermore, a trial of the NVX-CoV2373 vaccine (Novavax) showed 51.0% efficacy against the beta variant.20 Finally, high levels of neutralization have been seen with the P.1 (gamma) variant in serum samples obtained from persons vaccinated with the BNT162b2 vaccine, and one study showed only minimally reduced vaccine effectiveness against test-positive cases with one dose of messenger RNA vaccine.19,21,22
The delta variant is characterized by the spike protein mutations T19R, Δ157-158, L452R, T478K, D614G, P681R, and D950N.1 Several of these mutations may affect immune responses directed toward the key antigenic regions of receptor-binding protein (452 and 478) and deletion of part of the N-terminal domain.23 P681R is at the S1–S2 cleavage site, and it appears that strains with mutations at that site may have increased replication, which leads to higher viral loads and increased transmission.24 Data on the effectiveness of Covid-19 vaccines against clinical outcomes with this variant have been limited. In this study, we aimed to estimate the effectiveness of two Covid-19 vaccines, BNT162b2 and ChAdOx1 nCoV-19 (AstraZeneca), against symptomatic disease caused by the delta variant.
Methods
Study Design
We used two approaches to estimate the effect of vaccination on the delta variant. First, we used a test-negative case–control design to estimate vaccine effectiveness against symptomatic disease caused by the delta variant, as compared with the alpha variant, over the period that the delta variant has been circulating. This approach has been described in detail elsewhere.10 In brief, we compared vaccination status in persons with symptomatic Covid-19 with vaccination status in persons who reported symptoms but had a negative test. This approach helps to control for biases related to health-seeking behavior, access to testing, and case ascertainment.
For the secondary analysis, the proportion of persons with cases caused by the delta variant relative to the main circulating virus (the alpha variant) was estimated according to vaccination status. The underlying assumption was that if the vaccine had some efficacy and was equally effective against each variant, a similar proportion of cases with either variant would be expected in unvaccinated persons and in vaccinated persons. Conversely, if the vaccine was less effective against the delta variant than against the alpha variant, then the delta variant would be expected to make up a higher proportion of cases occurring more than 3 weeks after vaccination than among unvaccinated persons. Details of this analysis are described in Section S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org. The authors vouch for the accuracy and completeness of the data and for the fidelity of the trial to the protocol.
Data Sources
Vaccination Status
Data on all persons in England who have been vaccinated with Covid-19 vaccines are available in a national vaccination register (the National Immunisation Management System). Data regarding vaccinations that had occurred up to May 30, 2021, including the date of receipt of each dose of vaccine and the vaccine type, were extracted on June 1, 2021. Vaccination status was categorized as receipt of one dose of vaccine among persons who had symptom onset occurring 21 days or more after receipt of the first dose up to the day before the second dose was received, as receipt of the second dose among persons who had symptom onset occurring 14 days or more after receipt of the second dose, and as receipt of the first or second dose among persons with symptom onset occurring 21 days or more after the receipt of the first dose (including any period after the receipt of the second dose).
SARS-CoV-2 Testing
Polymerase-chain-reaction (PCR) testing for SARS-CoV-2 in the United Kingdom is undertaken by hospital and public health laboratories, as well as by community testing with the use of drive-through or at-home testing, which is available to anyone with symptoms consistent with Covid-19 (high temperature, new continuous cough, or loss or change in sense of smell or taste). Data on all positive PCR tests between October 26, 2020, and May 30, 2021, were extracted. Data on all recorded negative community tests among persons who reported symptoms were also extracted for the test-negative case–control analysis. Children younger than 16 years of age as of March 21, 2021, were excluded. Data were restricted to persons who had reported symptoms, and only persons who had undergone testing within 10 days after symptom onset were included, in order to account for reduced sensitivity of PCR testing beyond this period.25
Identification of Variant
Whole-genome sequencing was used to identify the delta and alpha variants. The proportion of all positive samples that were sequenced increased from approximately 10% in February 2021 to approximately 60% in May 2021.4 Sequencing is undertaken at a network of laboratories, including the Wellcome Sanger Institute, where a high proportion of samples has been tested, and whole-genome sequences are assigned to Public Health England definitions of variants on the basis of mutations.26
Spike gene target status on PCR was used as a second approach for identifying each variant. Laboratories used the TaqPath assay (Thermo Fisher Scientific) to test for three gene targets: spike (S), nucleocapsid (N), and open reading frame 1ab (ORF1ab). In December 2020, the alpha variant was noted to be associated with negative testing on the S target, so S target–negative status was subsequently used as a proxy for identification of the variant. The alpha variant accounts for between 98% and 100% of S target–negative results in England. Among sequenced samples that tested positive for the S target, the delta variant was in 72.2% of the samples in April 2021 and in 93.0% in May (as of May 12, 2021).4 For the test-negative case–control analysis, only samples that had been tested at laboratories with the use of the TaqPath assay were included.
Data Linkage
The three data sources described above were linked with the use of the National Health Service number (a unique identifier for each person receiving medical care in the United Kingdom). These data sources were also linked with data on the patient’s date of birth, surname, first name, postal code, and specimen identifiers and sample dates.
Covariates
Multiple covariates that may be associated with the likelihood of being offered or accepting a vaccine and the risk of exposure to Covid-19 or specifically to either of the variants analyzed were also extracted from the National Immunisation Management System and the testing data. These data included age (in 10-year age groups), sex, index of multiple deprivation (a national indication of level of deprivation that is based on small geographic areas of residence,27 assessed in quintiles), race or ethnic group, care home residence status, history of foreign travel (i.e., outside the United Kingdom or Ireland), geographic region, period (calendar week), health and social care worker status, and status of being in a clinically extremely vulnerable group.28 In addition, for the test-negative case–control analysis, history of SARS-CoV-2 infection before the start of the vaccination program was included. Persons were considered to have traveled if, at the point of requesting a test, they reported having traveled outside the United Kingdom and Ireland within the preceding 14 days or if they had been tested in a quarantine hotel or while quarantining at home. Postal codes were used to determine the index of multiple deprivation, and unique property-reference numbers were used to identify care homes.29
Statistical Analysis
For the test-negative case–control analysis, logistic regression was used to estimate the odds of having a symptomatic, PCR-confirmed case of Covid-19 among vaccinated persons as compared with unvaccinated persons (control). Cases were identified as having the delta variant by means of sequencing or if they were S target–positive on the TaqPath PCR assay. Cases were identified as having the alpha variant by means of sequencing or if they were S target–negative on the TaqPath PCR assay.
If a person had tested positive on multiple occasions within a 90-day period (which may represent a single illness episode), only the first positive test was included. A maximum of three randomly chosen negative test results were included for each person. Negative tests in which the sample had been obtained within 3 weeks before a positive result or after a positive result could have been false negatives; therefore, these were excluded. Tests that had been administered within 7 days after a previous negative result were also excluded. Persons who had previously tested positive before the analysis period were also excluded in order to estimate vaccine effectiveness in fully susceptible persons. All the covariates were included in the model as had been done with previous test-negative case–control analyses, with calendar week included as a factor and without an interaction with region.
With regard to S target–positive or –negative status, only persons who had tested positive on the other two PCR gene targets were included. Assignment to the delta variant on the basis of S target status was restricted to the week commencing April 12, 2021, and onward in order to aim for high specificity of S target–positive testing for the delta variant.4
Vaccine effectiveness for the first dose was estimated among persons with a symptom-onset date that was 21 days or more after receipt of the first dose of vaccine, and vaccine effects for the second dose were estimated among persons with a symptom-onset date that was 14 days or more after receipt of the second dose. Comparison was made with unvaccinated persons and with persons who had symptom onset in the period of 4 to 13 days after vaccination in order to help account for differences in underlying risk of infection. The period from the day of vaccine administration (day 0) to day 3 was excluded because reactogenicity to the vaccine can cause an increase in testing that biases results, as previously described.10
Results
Data Linkage
Among all the sequenced samples that were linked to the SARS-CoV-2 testing data set, 92.9% were linked to data on vaccination status. Over the course of the study period, there were 38,592 linked sequenced tests. In an analysis that was restricted to including only persons at least 16 years of age who had symptomatic Covid-19 caused by the alpha or delta variant and who had been vaccinated with either ChAdOx1 nCoV-19 or BNT162b2 according to an appropriate schedule, 19,109 sequenced cases were included (Fig. S1 in the Supplementary Appendix). The alpha variant was detected in 14,837 samples, and the delta variant in 4272 samples.
Descriptive Characteristics
The characteristics of persons with Covid-19 in the study population according to variant are shown in Table 1. Key differences with the delta variant included a higher proportion of persons with a history of foreign travel; a higher proportion of persons with cases in the most recent weeks (calendar weeks 18 to 20); a higher proportion of persons with cases in the northwest region, London, and the east of England; and a higher proportion of persons in the “Indian or British Indian,” “Pakistani or British Pakistani,” or “any other Asian background” ethnic groups. Little difference in the distribution of age or index of multiple deprivation was seen. Few cases of either variant were seen in persons older than 70 years of age, and only nine cases (all of which were with the alpha variant) occurred among care home residents.
Table 1

| Characteristic | Alpha Variant (N=14,837) |
Delta Variant (N=4272) |
Total (N=19,109) |
|---|---|---|---|
| Percent of total cases | 77.6 | 22.4 | 100 |
| Age — no. (%) | |||
| 16–29 yr | 5,325 (35.9) | 1571 (36.8) | 6,896 (36.1) |
| 30–39 yr | 4,199 (28.3) | 1164 (27.2) | 5,363 (28.1) |
| 40–49 yr | 2,923 (19.7) | 834 (19.5) | 3,757 (19.7) |
| 50–59 yr | 1,532 (10.3) | 465 (10.9) | 1,997 (10.5) |
| 60–69 yr | 657 (4.4) | 178 (4.2) | 835 (4.4) |
| 70–79 yr | 163 (1.1) | 47 (1.1) | 210 (1.1) |
| ≥80 yr | 38 (0.3) | 13 (0.3) | 51 (0.3) |
| History of travel — no. (%)† | |||
| No | 14,689 (99.0) | 4219 (98.8) | 18,908 (98.9) |
| Yes | 100 (0.7) | 52 (1.2) | 152 (0.8) |
| Unknown | 48 (0.3) | 1 (<0.1) | 49 (0.3) |
| Week that sample was obtained — no. (%)‡ | |||
| 14 | 3,316 (22.3) | 19 (0.4) | 3,335 (17.5) |
| 15 | 2,780 (18.7) | 53 (1.2) | 2,833 (14.8) |
| 16 | 2,517 (17.0) | 184 (4.3) | 2,701 (14.1) |
| 17 | 2,156 (14.5) | 372 (8.7) | 2,528 (13.2) |
| 18 | 1,775 (12.0) | 737 (17.3) | 2,512 (13.1) |
| 19 | 1,263 (8.5) | 1111 (26.0) | 2,374 (12.4) |
| 20 | 1,030 (6.9) | 1796 (42.0) | 2,826 (14.8) |
| Week of symptom onset — no. (%)‡ | |||
| 12 | 28 (0.2) | 0 | 28 (0.1) |
| 13 | 1,431 (9.6) | 8 (0.2) | 1,439 (7.5) |
| 14 | 3,089 (20.8) | 26 (0.6) | 3,115 (16.3) |
| 15 | 2,547 (17.2) | 89 (2.1) | 2,636 (13.8) |
| 16 | 2,381 (16.0) | 230 (5.4) | 2,611 (13.7) |
| 17 | 1,965 (13.2) | 501 (11.7) | 2,466 (12.9) |
| 18 | 1,622 (10.9) | 917 (21.5) | 2,539 (13.3) |
| 19 | 1,178 (7.9) | 1311 (30.7) | 2,489 (13.0) |
| 20 | 596 (4.0) | 1190 (27.9) | 1,786 (9.3) |
| Sex — no. (%) | |||
| Female | 7,681 (51.8) | 2047 (47.9) | 9,728 (50.9) |
| Male | 7,151 (48.2) | 2222 (52.0) | 9,373 (49.1) |
| Missing data | 5 (<0.1) | 3 (0.1) | 8 (<0.1) |
| Index of multiple deprivation — no. (%)§ | |||
| 1 | 4,780 (32.2) | 1446 (33.8) | 6,226 (32.6) |
| 2 | 3,302 (22.3) | 950 (22.2) | 4,252 (22.3) |
| 3 | 2,592 (17.5) | 654 (15.3) | 3,246 (17.0) |
| 4 | 2,302 (15.5) | 687 (16.1) | 2,989 (15.6) |
| 5 | 1,828 (12.3) | 524 (12.3) | 2,352 (12.3) |
| Missing data | 33 (0.2) | 11 (0.3) | 44 (0.2) |
| Clinically extremely vulnerable group — no. (%)¶ | |||
| No | 14,582 (98.3) | 4211 (98.6) | 18,793 (98.3) |
| Yes | 255 (1.7) | 61 (1.4) | 316 (1.7) |
| Care home resident — no. (%) | |||
| No | 14,828 (99.9) | 4272 (100) | 19,100 (100) |
| Yes | 9 (0.1) | 0 | 9 (<0.1) |
| Health or social care worker — no. (%) | |||
| No | 14,621 (98.5) | 4181 (97.9) | 18,802 (98.4) |
| Yes | 216 (1.5) | 91 (2.1) | 307 (1.6) |
| Race or ethnic group — no. (%)‖ | |||
| Bangladeshi or British Bangladeshi | 230 (1.6) | 98 (2.3) | 328 (1.7) |
| Chinese | 54 (0.4) | 18 (0.4) | 72 (0.4) |
| Indian or British Indian | 458 (3.1) | 705 (16.5) | 1,163 (6.1) |
| Pakistani or British Pakistani | 1,024 (6.9) | 510 (11.9) | 1,534 (8.0) |
| Any other Asian background | 278 (1.9) | 188 (4.4) | 466 (2.4) |
| Black African or Caribbean | 277 (1.9) | 113 (2.6) | 390 (2.0) |
| White | 9,662 (65.1) | 1801 (42.2) | 11,463 (60.0) |
| Mixed | 234 (1.6) | 71 (1.7) | 305 (1.6) |
| Any other ethnic group | 442 (3.0) | 139 (3.3) | 581 (3.0) |
| Missing data | 2,178 (14.7) | 629 (14.7) | 2,807 (14.7) |
| Region — no. (%) | |||
| East Midlands | 1,822 (12.3) | 380 (8.9) | 2,202 (11.5) |
| East of England | 1,178 (7.9) | 510 (11.9) | 1,688 (8.8) |
| London | 1,062 (7.2) | 536 (12.5) | 1,598 (8.4) |
| Northeast | 977 (6.6) | 69 (1.6) | 1046 (5.5) |
| Northwest | 2,664 (18.0) | 2138 (50.0) | 4,802 (25.1) |
| Southeast | 847 (5.7) | 198 (4.6) | 1045 (5.5) |
| Southwest | 198 (1.3) | 63 (1.5) | 261 (1.4) |
| West Midlands | 1,538 (10.4) | 241 (5.6) | 1,779 (9.3) |
| Yorkshire and Humber | 4,550 (30.7) | 135 (3.2) | 4,685 (24.5) |
| Missing data | 1 (<0.1) | 2 (<0.1) | 3 (<0.1) |
Characteristics of Persons with Covid-19 in the United Kingdom, According to Variant.*
*
B.1.1.7 is the alpha variant, and B.1.617.2 the delta variant, of the severe acute respiratory syndrome coronavirus 2, the virus that causes coronavirus disease 2019 (Covid-19). Percentages may not total 100 because of rounding.
†
Persons were considered to have traveled if, at the point of requesting a test, they reported having traveled outside the United Kingdom and Ireland within the preceding 14 days or if they had been tested in a quarantine hotel or while quarantining at home.
‡
The week number is the calendar week in 2021.
§
The index of multiple deprivation is a national indicator of level of deprivation on the basis of small geographic areas of residence; the index ranges from 1 (least deprived) to 5 (most deprived).27
¶
The status of being in a clinically extremely vulnerable group was defined according to NHS Digital.28
‖
Race or ethnic group was determined from data in the National Immunisation Management System register.
Among sequenced samples that were originally tested with the use of the TaqPath assay, a high correlation was seen between S target status and the two variants under investigation, with 95.3% of the S target–positive cases identified as having the delta variant and 99.6% of the S target–negative cases identified as having the alpha variant (Tables S1 and S2). The distribution of intervals between the receipt of vaccine doses is shown in Figure S2.
Vaccine Effectiveness Estimates
Results of the test-negative case–control analysis are shown in Table 2 and Figure 1. In the “any vaccine” analysis, in which data from the persons who received either vaccine were pooled, effectiveness was notably lower after the first vaccine dose among persons with the delta variant (30.7%; 95% confidence interval [CI], 25.2 to 35.7) than among those with the alpha variant (48.7%; 95% CI, 45.5 to 51.7). Results for the first dose were similar for both vaccines, with an absolute difference in vaccine effectiveness against the delta variant as compared with the alpha variant of 11.9 percentage points with the BNT162b2 vaccine and 18.7 percentage points with the ChAdOx1 nCoV-19 vaccine.
Figure 1

Vaccine Effectiveness against the Alpha and Delta Variants, According to Dose and Vaccine Type.
Shown is the effectiveness of one dose and two doses of the BNT162b2 and ChAdOx1 nCoV-19 vaccines, or either vaccine (“any”), against symptomatic disease with the B.1.1.7 (alpha) or B.1.617.2 (delta) variant of the severe acute respiratory syndrome coronavirus 2. 𝙸 bars indicate 95% confidence intervals.
Table 2

| Vaccination Status | Test-Negative Status | Alpha Variant or S Target–Negative Status |
Delta Variant or S Target–Positive Status |
||||
|---|---|---|---|---|---|---|---|
| Controls | Cases | Case:Control Ratio |
Adjusted Vaccine Effectiveness (95% CI) |
Cases | Case:Control Ratio |
Adjusted Vaccine Effectiveness (95% CI) |
|
| no. | no. | % | no. | % | |||
| Unvaccinated | 96,371 | 7313 | 0.076 | Reference | 4043 | 0.042 | Reference |
| Any vaccine | |||||||
| Dose 1 | 51,470 | 2226 | 0.043 | 48.7 (45.5–51.7) | 1493 | 0.029 | 30.7 (25.2–35.7) |
| Dose 2 | 23,993 | 143 | 0.006 | 87.5 (85.1–89.5) | 340 | 0.014 | 79.6 (76.7–82.1) |
| BNT162b2 vaccine | |||||||
| Dose 1 | 8,641 | 450 | 0.052 | 47.5 (41.6–52.8) | 137 | 0.016 | 35.6 (22.7–46.4) |
| Dose 2 | 15,749 | 49 | 0.003 | 93.7 (91.6–95.3) | 122 | 0.008 | 88.0 (85.3–90.1) |
| ChAdOx1 nCoV-19 vaccine | |||||||
| Dose 1 | 42,829 | 1776 | 0.041 | 48.7 (45.2–51.9) | 1356 | 0.032 | 30.0 (24.3–35.3) |
| Dose 2 | 8,244 | 94 | 0.011 | 74.5 (68.4–79.4) | 218 | 0.026 | 67.0 (61.3–71.8) |
Vaccine Effectiveness against the Alpha Variant or S Target–Negative Status and the Delta Variant or S Target–Positive Status, According to Dose and Vaccine Type.*
*
The adjusted analysis of vaccine effectiveness was adjusted for period (calendar week), travel history, race or ethnic group, sex, age, index of multiple deprivation, clinically extremely vulnerable group, region, history of positive test, health or social care worker, and care home residence. CI denotes confidence interval.
The difference in vaccine effectiveness was much smaller among persons who had received the second dose of vaccine. In the “any vaccine” analysis, the vaccine effectiveness was 87.5% (95% CI, 85.1 to 89.5) with the alpha variant and 79.6% (95% CI, 76.7 to 82.1) with the delta variant. With the BNT162b2 vaccine, a small difference in effectiveness between variants was seen after the second dose: 93.7% (95% CI, 91.6 to 95.3) with the alpha variant and 88.0% (95% CI, 85.3 to 90.1) with the delta variant. The effectiveness with two doses of the ChAdOx1 nCoV-19 vaccine was lower than with the BNT162b2 vaccine; however, with the ChAdOx1 nCoV-19 vaccine, the difference in effectiveness between the alpha and delta variants was small (74.5% [95% CI, 68.4 to 79.4] and 67.0% [95% CI, 61.3 to 71.8], respectively).
Table S3, in which the period after the first dose is stratified according to the period of 21 to 55 days and the period of 56 or more days, shows a possible indication of waning efficacy against the alpha variant with the BNT162b2 vaccine and against the delta variant with the ChAdOx1 nCoV-19 vaccine. Section S1 and Tables S4 through S6 show the results of the secondary analysis.
Discussion
We found that the absolute difference in vaccine effectiveness against symptomatic disease with one dose of vaccine with the delta variant as compared with the alpha variant was approximately 12 to 19 percentage points. However, the differences in vaccine effectiveness after two doses were small. This was the case for both the BNT162b2 and ChAdOx1 nCoV-19 vaccines. In the test-negative case–control analysis, the estimated vaccine effectiveness against symptomatic disease with the delta variant was approximately 36% with a single dose of the BNT162b2 vaccine and approximately 30% with a single dose of the ChAdOx1 nCoV-19 vaccine; the effectiveness was approximately 88% with two doses of the BNT162b2 vaccine and approximately 67% with two doses of the ChAdOx1 nCoV-19 vaccine.
A clear effect was noted with both vaccines, with high levels of effectiveness after two doses. Vaccine effectiveness against either variant was smaller after the receipt of two doses of the ChAdOx1 nCoV-19 vaccine than after the receipt of two doses of the BNT162b2 vaccine, a finding that is consistent with reported clinical trial findings.7,8 Differences between the two vaccines are further discussed in Section S2. The numbers of cases and follow-up periods are currently insufficient for the estimation of vaccine effectiveness against severe disease, including hospitalization and death.
One study from India that reported neutralization data in the broader B.1.617 variant category suggested that convalescent serum samples from persons with Covid-19 and from recipients of the BBV152 vaccine (Covaxin) were able to neutralize variants in the B.1.617 lineage.30 As compared with recent findings from Qatar on the effectiveness of the BNT162b2 vaccine against the alpha and beta variants,17 our findings suggest that effectiveness against the delta variant after a full vaccination course lies somewhere between these two. A comparison with previously reported estimates of vaccine effectiveness against the alpha variant is discussed in Section S2.
The large scale of testing and whole-genome sequencing in the United Kingdom, as well as the recording of vaccination status in a national vaccination register, allowed us to analyze vaccine effectiveness within a few weeks of the delta variant first emerging in the United Kingdom. We used two distinct analytic approaches that gave broadly similar results, and findings with our control analysis (using the alpha variant) are consistent with those that have been reported previously.7,8,10,17 Findings were also similar to those in cases that occurred during the first 2 weeks after receipt of the first vaccine dose (Table S4), which helps to rule out unmeasured confounders associated with both the likelihood of being vaccinated and the likelihood of being exposed to a variant. The use of a test-negative case–control design helped us to control for differences in health-seeking behavior between vaccinated persons and unvaccinated persons.
Our study has several limitations. The findings are observational and should be interpreted with caution. Low sensitivity or specificity of PCR testing could result in cases and controls being misclassified, which would attenuate the estimates of vaccine effectiveness. Low sensitivity or specificity of PCR testing could also affect one variant more than another, although this might be expected to affect the alpha variant more than the delta variant, given that, with an emerging variant, more cases may be detected earlier in infection, which may result in higher viral loads and increased sensitivity and specificity. Although we controlled for race or ethnic group, region, and an index of multiple deprivation, differences in vaccine coverage among population groups that may have more or less exposure to the delta variant may have affected the secondary analysis but should not have affected the test-negative case–control design. There may also be differences among the populations that received each vaccine — for example, in younger age groups, health care workers are more likely to have received the BNT162b2 vaccine, whereas persons in clinical risk groups are more likely to have received the ChAdOx1 nCoV-19 vaccine.11 Furthermore, the analysis also relied on the assumptions that any residual confounding in the test-negative case–control design would affect the two estimates of vaccine effectiveness equally or at least would not bias the adjusted odds ratio for the comparison of vaccine effectiveness for a given vaccine against the two variants; that is, the accuracy of the sequencing would not depend on the variant and the propensity among symptomatic persons to get tested would not differ according to variant.
Overall, we found high levels of vaccine effectiveness against symptomatic disease with the delta variant after the receipt of two doses. These estimates were only modestly lower than the estimate of vaccine effectiveness against the alpha variant. Our finding of reduced effectiveness after the first dose would support efforts to maximize vaccine uptake with two doses among vulnerable groups in the context of circulation of the delta variant.
Notes
Surveillance of coronavirus disease 2019 (Covid-19) testing and vaccination is undertaken under Regulation 3 of the Health Service (Control of Patient Information) Regulations 2002 to collect confidential patient information (www.legislation.gov.uk/uksi/2002/1438/regulation/3/made) under Sections 3(i) (a) to (c), 3(i)(d) (i) and (ii), and 3. The study protocol was subject to an internal review by the Public Health England Research Ethics and Governance Group and was found to be fully compliant with all regulatory requirements. Given that no regulatory issues were identified and that ethics review is not a requirement for this type of work, it was decided that a full ethics review would not be necessary.
This article was published on July 21, 2021, and updated on October 7, 2021, at NEJM.org.
Supported by Public Health England (PHE). The Covid-19 Genomics U.K. Consortium (COG-UK) is supported by funding from the Medical Research Council part of U.K. Research and Innovation, the National Institute of Health Research, and Genome Research, operating as the Wellcome Sanger Institute.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank the members of the PHE Covid-19 Data Science Team, the PHE Outbreak Surveillance Team, NHS England, NHS Digital, and NHS Test and Trace for their roles in developing and managing the testing for severe acute respiratory coronavirus 2 (SARS-CoV-2), variant identification and vaccination systems, and data sets, as well as the reporting NHS vaccinators and the staff of the NHS laboratories, PHE laboratories, and lighthouse laboratories; the staff of the Wellcome Sanger Institute and other laboratories that were involved in whole-genome sequencing of samples obtained from patients with Covid-19; the members of the Joint Committee on Vaccination and Immunisation and the U.K. Variant Technical Group for advice and feedback in developing this study; and Dr. Neil Ferguson for advice on the analysis.
Supplementary Material
References
1.
European Centre for Disease Prevention and Control. Threat assessment brief: emergence of SARS-CoV-2 B.1.617 variants in India and situation in the EU/EEA. May 11, 2021 (https://www.ecdc.europa.eu/en/publications-data/threat-assessment-emergence-sars-cov-2-b1617-variants).
2.
Rubin EJ, Baden LR, Udwadia ZF, Morrissey S. India’s Covid-19 crisis. N Engl J Med 2021;384(18):e84-e84.
3.
Elbe S, Buckland-Merrett G. Data, disease and diplomacy: GISAID’s innovative contribution to global health. Glob Chall 2017;1:33-46.
4.
Public Health England. SARS-CoV-2 variants of concern and variants under investigation in England. Technical briefing 11. May 13, 2021 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/986380/Variants_of_Concern_VOC_Technical_Briefing_11_England.pdf).
5.
Joint Committee on Vaccination and Immunisation. Priority groups for coronavirus (COVID-19) vaccination: advice from the JCVI, 30 December 2020. London: Department of Health and Social Care, January 6, 2021 (https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-30-december-2020).
6.
Joint Committee on Vaccination and Immunisation. Optimising the COVID-19 vaccination programme for maximum short-term impact. Independent report. London: Department of Health and Social Care, January 26, 2021 (https://www.gov.uk/government/publications/prioritising-the-first-covid-19-vaccine-dose-jcvi-statement/optimising-the-covid-19-vaccination-programme-for-maximum-short-term-impact).
7.
Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020;383:2603-2615.
8.
Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021;397:99-111.
9.
Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2021;384:403-416.
10.
Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ 2021;373:n1088-n1088.
11.
Hall VJ, Foulkes S, Saei A, et al. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study. Lancet 2021;397:1725-1735.
12.
Shrotri M, Krutikov M, Palmer T, et al. Vaccine effectiveness of the first dose of ChAdOx1 nCoV-19 and BNT162b2 against SARS-CoV-2 infection in residents of long-term care facilities (VIVALDI study). March 26, 2021 (https://www.medrxiv.org/content/10.1101/2021.03.26.21254391v1). preprint.
13.
Thompson MG, Burgess JL, Naleway AL, et al. Interim estimates of vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines in preventing SARS-CoV-2 infection among health care personnel, first responders, and other essential and frontline workers — eight U.S. locations, December 2020–March 2021. MMWR Morb Mortal Wkly Rep 2021;70:495-500.
14.
Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021;384:1412-1423.
15.
Vasileiou E, Simpson CR, Robertson C, et al. Effectiveness of first dose of COVID-19 vaccines against hospital admissions in Scotland: national prospective cohort study of 5.4 million people. February 19, 2021 (https://ssrn.com/abstract=3789264). preprint.
16.
Hyams C, Marlow R, Maseko Z, et al. Assessing the effectiveness of BNT162b2 and ChAdOx1nCoV-19 COVID-19 vaccination in prevention of hospitalisations in elderly and frail adults: a single centre test negative case-control study. March 3, 2021 (https://ssrn.com/abstract=3796835). preprint.
17.
Abu-Raddad LJ, Chemaitelly H, Butt AA. Effectiveness of the BNT162b2 Covid-19 vaccine against the B.1.1.7 and B.1.351 variants. N Engl J Med 2021;385:187-189.
18.
Wang P, Nair MS, Liu L, et al. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature 2021;593:130-135.
19.
Liu Y, Liu J, Xia H, et al. Neutralizing activity of BNT162b2-elicited serum. N Engl J Med 2021;384:1466-1468.
20.
Shinde V, Bhikha S, Hoosain Z, et al. Efficacy of NVX-CoV2373 Covid-19 vaccine against the B.1.351 variant. N Engl J Med 2021;384:1899-1909.
21.
Parry HM, Tut G, Faustini S, et al. BNT162b2 vaccination in people over 80 years of age induces strong humoral immune responses with cross neutralisation of P.1 Brazilian variant. March 31, 2021 (https://ssrn.com/abstract=3816840). preprint.
22.
Skowronski DM, Setayeshgar S, Zou M, et al. Single-dose mRNA vaccine effectiveness against SARS-CoV-2, including P.1 and B.1.1.7 variants: a test-negative design in adults 70 years and older in British Columbia, Canada. June 9, 2021 (https://www.medrxiv.org/content/10.1101/2021.06.07.21258332v1). preprint.
23.
Li Q, Wu J, Nie J, et al. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell 2020;182(5):1284.e9-1294.e9.
24.
Johnson BA, Xie X, Kalveram B, et al. Furin cleavage site is key to SARS-CoV-2 pathogenesis. August 26, 2020 (https://www.biorxiv.org/content/10.1101/2020.08.26.268854v1). preprint.
25.
Singanayagam A, Patel M, Charlett A, et al. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill 2020;25:2001483-2001483.
26.
Bull M, Chand M, Connor T, et al. Standardised variant definitions. 2021 (https://github.com/phe-genomics/variant_definitions).
27.
Ministry of Housing, Communities, and Local Government. English indices of deprivation 2019. September 26, 2019 (https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019).
28.
NHS Digital. COVID-19 — high risk shielded patient list identification methodology: rule logic. 2020 (https://digital.nhs.uk/coronavirus/shielded-patient-list/methodology/rule-logic).
29.
Care Quality Commission. CQC care directory. 2021 (https://www.cqc.org.uk/files/cqc-care-directory-zip).
30.
Yadav PD, Sapkal GN, Abraham P, et al. Neutralization of variant under investigation B.1.617 with sera of BBV152 vaccinees. April 23, 2021 (https://www.biorxiv.org/content/10.1101/2021.04.23.441101v1). preprint.
Information & Authors
Information
Published In
Copyright
Copyright © 2021 Massachusetts Medical Society. All rights reserved.
History
Published online: July 21, 2021
Published in issue: August 12, 2021
Topics
Authors
Affiliations
From Public Health England (J.L.B., N.A., C.G., E.G., R.S., S.T., J.S., E.T., N.G., G.D., R.M., C.N.J.C., G.A., M.E., M.Z., K.E.B., S.H., M.C., M.R.), the National Institute of Health Research (NIHR) Health Protection Research Unit in Vaccines and Immunisation, London School of Hygiene and Tropical Medicine (J.L.B., N.A., C.N.J.C., G.A., K.E.B., M.R.), the NIHR Health Protection Research Unit in Respiratory Infections, Imperial College London (J.L.B., M.Z.), and Guy’s and St. Thomas’ Hospital NHS Trust (M.C.), London, and Healthcare Associated Infections and Antimicrobial Resistance, University of Oxford, Oxford (S.H.) — all in the United Kingdom.
Metrics & Citations
Metrics
Altmetrics
Citations
Export citation
Select the format you want to export the citation of this publication.
Cited by
- Magnitude and Duration of Serum Neutralizing Antibody Titers Induced by a Third mRNA COVID-19 Vaccination against Omicron BA.1 in Older Individuals, Infection & Chemotherapy, 56, 1, (25), (2024).https://doi.org/10.3947/ic.2023.0057
- Short-Term Adverse Effects of the Fourth Dose of Vaccination against COVID-19 in Adults over 40 Years of Age, Vaccines, 12, 4, (400), (2024).https://doi.org/10.3390/vaccines12040400
- Safety and Immunogenicity of the Monovalent Omicron XBB.1.5-Adapted BNT162b2 COVID-19 Vaccine in Individuals ≥12 Years Old: A Phase 2/3 Trial, Vaccines, 12, 2, (118), (2024).https://doi.org/10.3390/vaccines12020118
- Association between COVID-19 Vaccination and SARS-CoV-2 Infection among Household Contacts of Infected Individuals: A Prospective Household Study in England, Vaccines, 12, 2, (113), (2024).https://doi.org/10.3390/vaccines12020113
- The Immunogenicity of CpG, MF59-like, and Alum Adjuvant Delta Strain Inactivated SARS-CoV-2 Vaccines in Mice, Vaccines, 12, 1, (60), (2024).https://doi.org/10.3390/vaccines12010060
- Predicting Vaccine Effectiveness for Hospitalization and Symptomatic Disease for Novel SARS-CoV-2 Variants Using Neutralizing Antibody Titers, Viruses, 16, 3, (479), (2024).https://doi.org/10.3390/v16030479
- The Nucleocapsid Protein of SARS-CoV-2, Combined with ODN-39M, Is a Potential Component for an Intranasal Bivalent Vaccine with Broader Functionality, Viruses, 16, 3, (418), (2024).https://doi.org/10.3390/v16030418
- Exploring the Interplay between COVID-19 and Gut Health: The Potential Role of Prebiotics and Probiotics in Immune Support, Viruses, 16, 3, (370), (2024).https://doi.org/10.3390/v16030370
- Causes and Consequences of Coronavirus Spike Protein Variability, Viruses, 16, 2, (177), (2024).https://doi.org/10.3390/v16020177
- Whole-Genome Sequencing and Mutation Analyses of SARS-CoV-2 Isolates from Indonesia, Pathogens, 13, 4, (279), (2024).https://doi.org/10.3390/pathogens13040279
- See more
Loading...